As LA makes all autopsy results public, a reader suggested I may be interesting in taking a look. It can be easy for memory and recall to change over time and I wondered whether it was possible one bottle of formula could have saved him. Whilst these cases are traumatic and difficult to discuss. It's vital we do so in order to minimise the risks of this happening to another child.
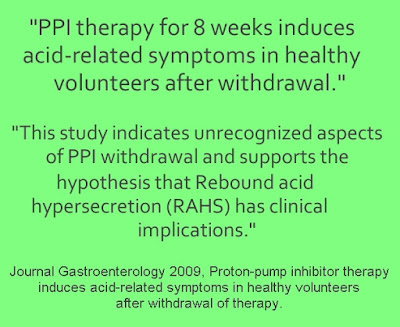
It's not exactly easy to pick this story apart, because errors appear to be present in the autopsy report:
- Page 15 and the opening summary, states baby's birth weight was 7lb 7 ounces (3.36 kg). It states in this same paragraph is records his discharge weight as 6lb 5 ounces (2.86 kg)
- Page 17 also states his discharge weight was 6lb 5 ounces (2.86 kg)
- Page 18 states that his discharge weight was 3.03 kg (6lb 11oz)
This is a significant discrepancy. The first gives a loss of 15%, the second a loss of 9.8% at day 4.
But what happened before then?
"Fetal intolerance to labor"
Labour progressed typically until epidural meds were given, at which point baby's heartbeat decreased. This didn't improve with maternal positioning and thus they ruptured mum's membranes to enable them to attach a monitor to baby. This showed baby still had a slow heartbeat and thus they moved to cesarean section.
Once Landon was born:
- Page 16, based on an interview with a doctor reviewing the case:
- Page 17, based on maternal interview:
- Page 18, based on official medical records
Causes of Hypovolemia are:
- Blood loss–from an injury or illness
- Problems absorbing fluids in the digestive tract
- Trouble feeding
- Illness with vomiting or diarrhea
Clearly since he was just born - feeding and vomiting etc can't apply.
All reports agree that just 2 hours later, Landon was discharged from the NICU to room in with his mother for the next four days.
They were taken to the maternity ward:
They were taken to the maternity ward:
"She [mum] had concerns because he was fussy, she thought he would sleep and eat more".
"During the hospital stay, baby appeared to be nursing, but mum raised concerns she didn't have enough milk due to a history of PCOS". The infant produced few wet diapers.
On day 4 baby was discharged at 3pm despite the fact baby had produced ZERO wet nappies that day and as we explored above, had a loss of either 10 or 15% at that point.
Once home Landon fed continuously. Mum states she was advised that this was normal as baby was cluster "feeding".
The report becomes a tad contradictory:
On day 4 baby was discharged at 3pm despite the fact baby had produced ZERO wet nappies that day and as we explored above, had a loss of either 10 or 15% at that point.
Once home Landon fed continuously. Mum states she was advised that this was normal as baby was cluster "feeding".
The report becomes a tad contradictory:
- Page 16 reads: the baby was home for 8-10 hours and was not feeding well. The father states the child had poor skin turgor. On the night in question they had called the hospital for advice and nobody suggested supplementation. The child was not doing well and so they were going to take him hospital.
- Page 18 reads: It was reported that the mother fell asleep breastfeeding the infant at 02:00 hours (no hospital visit). She woke 30-40 minutes later to find him blue and not breathing.
- In contrast posts online from mum recount how he slept in the car and then "they had fun playing with him that evening" yet awoke to find him unresponsive.
Rushed to hospital:
Baby was resuscitated, readmitted and rehydrated with IV fluids (noted by the pathologist to be visibly swollen due to the volume), at this point baby was 9.3% below birth-weight.
Medical professionals I've discussed this with have said if baby was discharged with a 9.8% loss, you'd typically expect a significant positive shift following IV fluids, particularly if baby looks oedematous. As we know from what happened to Dr Christie del Castillo-Hegyi of "Fed is Best" - we start seeing these dangerous sequale unfold when we start hitting these very large losses.
Medical professionals I've discussed this with have said if baby was discharged with a 9.8% loss, you'd typically expect a significant positive shift following IV fluids, particularly if baby looks oedematous. As we know from what happened to Dr Christie del Castillo-Hegyi of "Fed is Best" - we start seeing these dangerous sequale unfold when we start hitting these very large losses.
The picture painted by the media and groups trying to use this story to promote a formula feeding agenda - is so far away from reality, it's at best misleading and at worst lies intended to manipulate. Instead of a term, healthy baby apparently feeding well, with normal output and yet suddenly struck down (ie it could happen to anyone!), the reality is very different.
Baby Landon was dehydrated at birth with no explanation as to why since no excessive blood loss is noted. Following his NICU stay and subsequent rooming in, there are persistent warning signs this was a compromised baby unable to transfer enough colostrum to sustain himself. First mum states she thought baby was fussy and would have fed more - given this baby had just been discharged from NICU for dehydration, fussiness (which expends energy and suggests something is wrong) along with lack of feeding should surely have raised a red flag?
The report states during the hospital stay baby "appeared" to be feeding, yet mum was unsure if she was producing adequate milk and had concerns over PCOS and potential insufficient glandular tissue. What this tells us is mum's instincts are baby wasn't feeding well, yet it seems no action was taken by doctors caring for Landon to ensure he now remained adequately hydrated and able to feed well during his stay.
Babies can fail to latch effectively for a number of reasons but those most at risk of problems are babies in Landon's position. In fact on day 4, after continuing to lose weight during his stay, a dehydrated baby without adequate urine output was discharged from hospital. No feeding plan or safeguarding protocols were implemented and just hours late his mother fell asleep with him in arms.
If the baby had been bottle fed and mum had kept handing back full bottles of unused formula, would staff have been OK with this too? If not, it clearly demonstrates staff NEED the skills to identify when a baby is drinking well. They need to check and double check infants who have left NICU following dehydration (of all things!), weighing baby to plot against nomograms if needed
They NEED to listen to mothers who state their baby doesn't appear to be drinking well, is fussy, is never satisfied - these things are NOT normal!